Why Trauma Hijacks Your Rest and How to Reclaim It
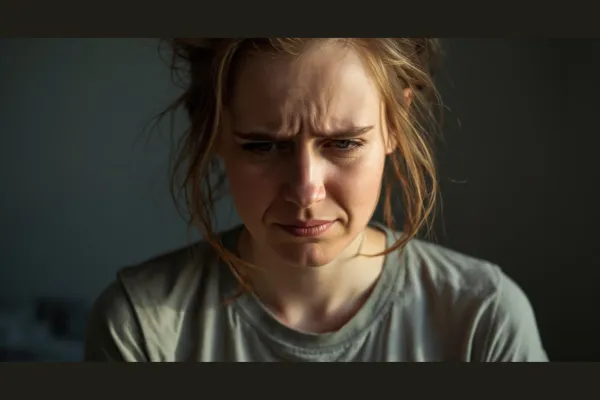
Do you wake up feeling exhausted, even after a full night’s sleep? What if I told you your past might be actively sabotaging your rest—every single night?
Today, we’re unpacking what I call the Sleep Paradox: the strange and deeply frustrating experience where the body is desperate for rest, yet the nervous system refuses to allow it.
And this is not a motivation issue. It is not a discipline issue. And it is definitely not a “just relax” issue.
It’s a nervous system issue.
For years, sleep felt like a battle I was constantly losing. I could be physically exhausted, mentally drained—and yet the moment my head hit the pillow, my system would shift into alert mode. Racing thoughts. Shallow breathing. A body that felt like it was bracing for impact instead of preparing for repair.
If you’ve ever felt like your body wants to rest but your system won’t let it, you’re not broken—and you’re not alone.
Here’s the core truth most people miss:
Sleep is not something you do. Sleep is something your nervous system allows.
And trauma fundamentally disrupts that permission.
Modern sleep science, including the work of Matthew Walker, shows us that sleep is the brain’s primary mechanism for emotional regulation, memory integration, immune repair, and nervous system recalibration.
During deep non-REM sleep, the brain performs physical restoration. During REM sleep, it performs emotional processing—decoupling emotional charge from memory content.
But here’s the paradox.
Trauma requires sleep to heal— yet trauma impairs the very neural conditions required for sleep.
Why?
Because trauma is not stored as a story. It is stored as unfinished survival physiology.
When the nervous system has learned—through lived experience—that it is not safe to fully power down, it remains sympathetically dominated. Heart rate stays slightly elevated. Cortisol rhythms flatten. The amygdala remains hypersensitive. And the brainstem continues scanning for threat.
Even in the dark. Even in silence. Even in bed.
So when night comes—the exact moment the nervous system is supposed to shift out of sympathetic vigilance and into parasympathetic repair—the system does the opposite.
It interprets stillness as danger.
That’s why people with unresolved trauma don’t just struggle to fall asleep.
They struggle to stay asleep. They wake from vivid dreams. They experience early-morning cortisol spikes. They wake feeling unrested, foggy, and emotionally raw.
Not because they slept “wrong.” But because their nervous system never made the parasympathetic transition.
This is where mainstream sleep advice completely misses the mark.
You cannot cognitively convince a sympathetically dominated nervous system to rest. You cannot positive-think your way into parasympathetic tone. And you cannot discipline a survival response into submission.
Sleep disruption after trauma is not psychological weakness. It is biological vigilance.
So how do we reclaim sleep—without reliving the past?
The answer is state regulation before sleep, not memory excavation during sleep.
The goal is not to analyze trauma at night. The goal is to shift the nervous system out of sympathetic dominance and into parasympathetic safety long enough for sleep architecture to re-emerge.
That begins with one critical understanding:
Your nervous system responds far more to sensory input and spatial orientation than to insight.
This is why visual-spatial tasking and rhythmic breathing work so well. They bypass the narrative brain and communicate directly with the midbrain and brainstem—the regions that decide whether parasympathetic activation is allowed.
Here are three principles that matter more than any sleep hack.
First: Downshift before bed becomes the battlefield.
If the first time your nervous system is asked to slow down is when the lights go off, you’re already too late. Regulation must begin earlier—through dimmer light, slower movement, reduced stimulation, and lower cognitive load.
This isn’t lifestyle advice. This is autonomic sequencing.
You’re teaching the system that nightfall does not equal threat.
Second: Replace rumination with orientation.
A sympathetically dominant nervous system collapses inward. It loops thoughts. It scans internally. It replays.
Orientation does the opposite.
Soft peripheral vision—widening your visual field instead of staring—signals safety to the brainstem. Slow spatial awareness tells the nervous system there is no immediate threat to track.
Safety is not a thought. It is a felt spatial condition.
Third: Use breath to actively stimulate parasympathetic tone
One of the simplest and most effective tools here is cyclic sighing: a double inhale through the nose, followed by a long, slow exhale through the mouth.
This pattern directly stimulates the vagal pathways associated with parasympathetic activation. It tells the body, “The threat response can stand down.”
Stillness becomes tolerable when it is paired with regulation.
And over time, the nervous system relearns something critical: Rest does not equal risk.
This is how sleep returns—not through effort, but through permission.
Now, one important piece most people never get taught.
If you wake up in the middle of the night, you are almost always waking from REM sleep. That doesn’t mean something went wrong. It means your brain was doing emotional processing.
What matters is what you do next.
If you wake during REM:
Stay lying down
Stay in the dark
Do not reach for your phone
Do not turn on bright light
Instead, gently shift into peripheral vision—even with your eyes closed—and use cyclic sighing to stimulate parasympathetic tone.
You are not trying to “sleep harder.” You are allowing the system to re-enter parasympathetic dominance.
Most people accidentally re-trigger sympathetic activation by sitting up, checking the time, or engaging cognition. Darkness, stillness, peripheral awareness, and breath keep the system oriented toward safety.
And when sleep begins to stabilize, something remarkable happens.
Emotional reactivity decreases. Cognitive clarity improves. Pain perception shifts. Memory integration resumes.
Sleep is not just recovery.
Sleep is neurobiological reconciliation.
The tragedy is that so many people believe their broken sleep is the problem—when in reality, it is the signal.
A message from a nervous system that adapted brilliantly once and now needs help standing down.
If trauma has disrupted your sleep, the path forward is not harder nights or deeper analysis.
It is smarter regulation.
Rest is not a luxury. It is a biological requirement. And it is reclaimable.
When the nervous system feels safe enough, sleep will do what it has always known how to do: repair, integrate, and restore.
That’s the paradox. And that’s the promise.
---
Learn something? Share the post with others, and follow me, Allen Kanerva , for more.
Want to learn more on healing trauma?
Subscribe to my YouTube community today: https://www.youtube.com/@allen.kanerva